“I’ve Been Told I Have Bone on Bone Osteoarthritis. How Can Physical Therapy Help?”
Traditional thought has lead us in the direction that the changes often seen on X-rays and MRIs have a direct relationship with pain. Arguably the most common of these changes is osteoarthritis, or more informally known as the dreaded “Bone on Bone” changes. This bone on bone boogey man has long been a backbone (pun?) in modern medicine and rehab as an explanation as to why pain exists and how it can be treated. But, recent research and the surge of pain neuroscience education or “PNE” has put this long held belief into question. These developments have identified a number of factors associated with a person’s pain experience. To name a few…
And to name a few more…
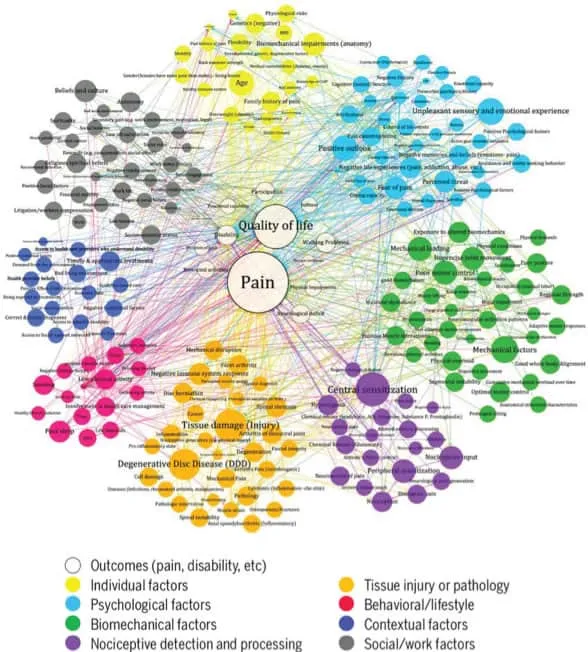
As you can see above, structural changes, like osteoarthritis (or “bone on bone”) offer just a piece to this continually evolving puzzle. As Greg Lehman, Physical Therapist, Chiropractor, and PNE expert puts it, “structure is not destiny”. In other words, those scary changes seen on an X-ray or MRI often do not predict what you can and cannot do, and should not steer you away from activities that are meaningful to you. Take a look at some of the research below which highlights the some of the points made above:
So pain is complex. Why should I care?
Because the nature of pain is so complex, there are multitude of ways in which pain can be treated…and treated effectively – many of which fall under what PT’s do on a day to day basis.
We understand at Universus Physical Therapy that there is no one size fits all approach to care, and embrace that fact.We take the time to look beyond just structure and identify the other drivers of pain that could be affecting your recovery and full return to function.
Key Points:
-
Pain is complex, but can be managed with a wide array of treatment interventions including, but not limited to: targeted exercise, manual therapy, and pain neuroscience education.
-
Structural changes like, “bone on bone” arthritic changes are unlikely the sole driver for your pain.
-
Age related changes seen on X-rays and MRIs should not dictate what you can and cannot do, especially the activities most meaningful to you.
References:
-
Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine. May 15th 2005; 30(10);1173-1180
-
Gignac MA, Davis AM, Hawker G, et al. “What do you expect? You’re just getting older” : A comparison of perceived osteoarthritis-related and aging-related health experiences in mid and old-age adults. Arthritis Rheum. Dec 15 2006; 55(6); 905-912
-
Thielke S, Sale K, Reid MC. Aging: are these 4 pain myths complicating care? J Fam Pract. Nov 2012; 61(11); 666-670.
-
DePaul a MJ, Ketchum JM, Saullo TR, Laplante BL. Is the history of a surgical discogenic related to the source of chronic low back pain? Pain physician. Jan-Feb 2012; 15(1); E53-58
-
Okada E, Matsumoto M, Fujiwara H, Toyama Y. Disc degeneration of cervical spine on MRI in patients with lumbar disc herniation; comparison study with asymptomatic volunteers. Eur Spine J. Apr 2011; 20(4); 585-591.
-
Munk B, Lundorf E, Jensen J. Long-term outcome of meniscal degeneration in the knee: poor association between MRI and symptoms in 45 patients followed more than 4 years. Acts Orthop Scand. Feb (2004); 75(1); 89-92.
-
Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC musculoskeletal disorders. 2008;9:116
-
Silvis ML, Mosher TJ, Smetana BS, et al. Prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. Apr 2011; 39(4):715-721